Specialist Podiatric Foot Surgeon
We specialise in the diagnosis and treatment of foot problems.
Advanced Foot Specialist in Shellharbour
South Coast Foot Surgery, part of the Relieve Health Group, offers world-class specialist care using advanced techniques and technologies to enable lifelong movement.
Our expert care includes both conservative and surgical treatment options for all foot conditions.

Specialist Foot Surgeon
Dr. Hungerford Welcomes All Patients, With And Without A Referral, For The Specialist Opinion Of All Foot Conditions. Come Visit Us In Shellharbour City To Get Started With Your Treatment.
An Advanced Practice Led by a Specialist Foot Surgeon
Dr. Hungerford, podiatric surgeon, strives for a seamless patient experience from diagnosis through to completion of treatment. If you suffer from foot deformity, are dealing with complex foot concerns or are experiencing foot pain, we are here to help you get better.
Dr. Kent Hungerford is a nationally registered Specialist Podiatric Surgeon through the Australian Health Practitioner Regulation Agency (AHPRA). He is a member of the Australasian College of Podiatric Surgeons (MACPS) and is a member of the Australian Podiatry Association (MAPodA).
Having undertaken training locally and abroad, Dr. Hungerford specialises in the surgical treatment of the foot with a focus on minimally invasive or keyhole foot surgery. This includes treatment for conditions such as bunions, hammertoes, heel pain, Morton’s neuroma, ingrown toenails, warts/verruca and many others.

What We Treat
Dr Kent Hungerford will take a detailed look at your medical history and symptoms and will thoroughly assess your feet to provide the necessary testing to ensure the most accurate diagnosis.
Click for more information.
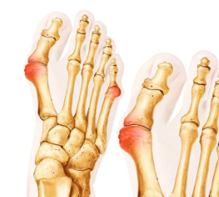
Bunion and Bunionette
A bunion, AKA hallux abductovalgus or hallux valgus, is a noticeable bump that emerges at the base of your big toe. This happens when some of the bones in the front part of your foot move out of place, causing your big toe to lean towards the others, which results in an outward protrusion of the joint. It can often lead to discomfort or pain, especially when walking or wearing shoes.
While bunions are often hereditary, they can also be exacerbated by wearing tight, narrow shoes and can cause inflammation, soreness, and potentially hinder your mobility.

By increasing the efficiency of the feet, ankles and legs we can decrease how fast your bunion or bunionette progresses in severity. This is typically undertaken through customised foot orthoses which increase muscle efficiency and spread your body weight throughout your whole foot. They may include accommodations to reduce pressure through the big toe joint. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Exercises can help to strengthen the small muscles within your foot to help correct your biomechanics. We recommend undertaking short footing, doming, toe curls and calf stretches.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that your bunion pain may be decreased. We recommend joggers or walking shoes when you’re undertaking activity to decrease the pressure on your toes. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease the pressure on your bunion and toes and increases the efficiency of your lower leg and foot muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot slipping forward. This will stop your foot and toes from moving forward and impacting your toes on the end of your shoe. Another great option is a bunion step-over lacing. This removes the pressure from your laces on the bunion bump, making you more comfortable almost immediately.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
When bunions and their associated pressure areas become a significant problem and are not able to be managed effectively through conservative options, surgery may be suggested.
Before surgery is undertaken a thorough assessment of your current health is required. This may involve discussion with your GP and specialists to ensure that surgery is safe for you to undertake.
Depending on the size of your bunion deformity and what your imaging including x-rays show, the procedure may be a more simple minimal incision surgery or it could be an open fusion of the big toe joint.
If you have pain or pressure from a bunion you may find information that can help, however, to learn more about options specific for you, book an appointment.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
Bunionettes are a prominence to the outside of your little toe joint. It can can be treated effectively with the above conservative management. When conservative options fail bunionette surgery can be undertaken. Particularly for younger and athletic patients, or anyone who is in pain, undertaking bunionette surgery whilst it is smaller will mean a quicker, more successful recovery.
Typically, bunionettes at this stage can be fixed by cutting through the fifth metatarsal bone just before the bump and moving it and your 5th toe towards the fourth toe. This is typcially undertaken without a screw or fixation and is held in palce with dressings and special post surgical tape.
This type of bunionette surgery is undertaken by minimal incision or keyhole surgery. Keyhole bunionnette surgery is an effective way to reduce your bunionette pain due t pressure and reduce your recovery time. Most patients will recover from minimal incision or keyhole bunionette surgery quickly.
Typical recovery is as follows:
Day 1 to week 1 – Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. A bit more activity up to 20minutes per hour to tolerance but no extended walking or activity. Continue foot elevation when seated or laying down. Activity related pain, bruising and swelling is normal.
Week 2 – Any stitches are taken out and compression bandage is put in place. Able to undertake upper body exercise. Able to return to work if office based where you are able to elevate the foot.
Week 4 – Progress review with surgeon and likely transition to joggers allowed. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 8 – Progress review with surgeon and return to higher impact sports as comfortable. Continue compression as required and can return to wedged shoes or small heel. Pain should have resolved and swelling is likely to be present, particularly on increased activity.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
Most times mild bunions can be treated effectively with the above conservative management. When conservative options fail bunion surgery can be undertaken. Particularly for younger and athletic patients, or anyone who is in pain, undertaking bunion surgery whilst it is smaller will mean a quicker, more successful recovery.
Typically, bunions at this stage can be fixed by reducing the bump and moving your big toe closer to your second toe. You may also require a bone cut to your big toe to place it in a more normal position. For this procedure, a screw is used to hold it in place.
This type of bunion surgery can be done open or by minimal incision or keyhole bunion surgery. Keyhole bunion surgery is an effective way to fix your bunion and reduce your recovery time. Most patients will recover from minimal incision or keyhole bunion surgery quickly.
Typical recovery is as follows:
Day 1 to week 1 – Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. A bit more activity up to 20minutes per hour to tolerance but no extended walking or activity. Continue foot elevation when seated or laying down. Activity related pain, bruising and swelling is normal.
Week 2 – Stitches are taken out and compression bandage put in place. Daily range of motion exercises provided. Able to undertake upper body exercise. Able to return to work if office based where you are able to elevate the foot.
Week 4 – Progress review with surgeon and likely transition to joggers allowed. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 8 – Progress review with surgeon and return to higher impact sports as comfortable. Continue compression and can return to wedged shoes or small heel. Pain should have resolved and swelling is likely to be present, particularly on increased activity.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
When a bunion deformity is larger, more corrective surgery is required. This may involve correction at your midfoot as well as at your big toe as per the mild bunion. You may also require a bone cut to your big toe to place it in a more appropriate position.
Typically, these bunion surgeries are undertaken open but depending on your case it may be able to be undertaken by minimal incision or keyhole bunion surgery.
Most patients will require a standard healing time with strict activity limitations.
Typical recovery is as follows:
Day 1 to week 1 – Dressings in place with a rigid-soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Waling with crutches required. Mild-moderate pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. Minimal activity restricted to home with foot elevation 80% of the time, able to do home-based activity with crutches. Continue foot elevation when seated. Mild pain, bruising and swelling is normal.
Week 2 to week 4 – Stitches taken out and compression bandage put in place at week 2. Move from crutches to walking however restricted to activity in the rigid soled post-operative sandal around home as tolerated.
Week 4 – Progress review with surgeon and likely transition to joggers allowed. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Able to undertake upper body exercises. Able to return to work if office-based where you are able to elevate the foot. Minimal pain and moderate swelling is normal.
Week 8 – Progress review with surgeon and return to all activity, except sport, as comfortable. Continue compression and can return to a wedged shoe or small heel. Pain should have resolved and swelling is likely to be mild, particularly on increased activity.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
In large bunion deformity, a more comprehensive procedure is required. This may include fusing your big toe joint or fusing the joint before your big toe joint. They may also include a mild or moderate bunion procedure.
These bunion surgeries are all undertaken open and require multiple screws and often a metal fixation plate.
Healing time is prolonged and strict activity limitations are necessary to ensure appropriate healing and long-term resolution of your bunion pain.
Typical recovery is as follows:
Day 1 to week 1 – Dressings in place with a rigid-soled post-operative sandal. Waling with crutches required, Minimal activity restricted to home with foot elevation 90% of the time. Mild-moderate pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. Minimal activity restricted to home with foot elevation 80% of the time, able to do minimal home-based activity. Continue foot elevation when seated. Mild pain, bruising and swelling is normal.
Week 2 to week 4 – Stitches taken out and compression bandage put in place at week 2. Restricted to activity in the rigid soled post-operative sandal around home as tolerated. Crutches may be stopped
Week 4 – Progress review with surgeon. Continued use of compression bandage. Able to return to work if office based where you are able to elevate the foot. Minimal pain and swelling is normal.
Week 6 – Progress review with surgeon and likely transition to joggers allowed. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
Hammertoe and Plantar Plate Tears
A hammertoe, claw toe, mallet toe is a foot condition where there’s an abnormal bend in the middle joint of one or more of your toes, causing them to resemble a hammer. This deformity can be a result of genetics or an injury to the plantar plate, a ligament that holds down your toe.
It is often seen in people with high or flat foot arches. It can cause discomfort or pain, especially when wearing shoes, and may also lead to the formation of corns, calluses and wounds on top of the joint or at the end of the toe.

Straight after injury or trauma, the toe should be splinted into a corrected position. This is undertaken using medical tape, silk tape or sports tape in a ribbon fashion to hold the toe down. By then taping the toe into a straight position, a hammertoe or claw toe will be corrected.
By increasing the efficiency of the feet, ankles and legs we can decrease how fast your hammertoe or claw toe progresses in severity. This is typically undertaken through customised foot orthoses which increase muscle efficiency and spread your body weight throughout your whole foot. They may include accommodations to remove pressure from an inflamed plantar plate tear as well as to move pressure away from prominent or painful areas. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Exercises can help to strengthen the small muscles within your foot to help correct your hammertoe or claw toe. We recommend undertaking short footing, doming, toe curls and calf stretches.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that your claw toe or hammertoe pain may be decreased. We recommend joggers or walking shoes when you’re undertaking activity to decrease the pressure on your toes. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease the pressure on your toes and increases the efficiency of your lower leg and foot muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot slipping forward. This will stop your foot and toes from moving forward and impacting your toes on the end of your shoe.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
When conservative options fail, hammertoes are managed surgically. The toes flexibility tells us the correct type of procedure that will give the best outcome for you with the least recovery time and impact on your life. When they are completely flexible a minimal incision, or keyhole hammertoe surgery undertaken in our rooms is very effective. When they are only partially flexible or unable to be moved, a minimal incision or keyhole hammertoe surgery is undertaken to provide you with the best outcome whilst preventing it from reoccurring.
Flexible hammertoes are managed by releasing a tendon that is too tight underneath your toe. This will reduce your toe into a corrected position. This procedure is undertaken via minimal incision or keyhole hammertoe surgery. The position is then maintained by taping it in position for several weeks whilst healing occurs.
Typical recovery is as follows:
Day 1 to day 4- Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation as much as possible. Mild pain and mild swelling is normal.
Day 4 to week 2- Dressings are changed and reduced. Able to return to work if office-based and able to elevate the foot. Able to do most home-based activity that does not involve prolonged standing. Continue foot elevation when seated. Mild pain and mild swelling is normal.
Week 2- Stitches are taken out (if used) and compression bandage put in place along with specific hammertoe taping instructions for the patient to undertake at home. Transition to joggers allowed. No pain and minimal swelling is normal.
Week 4- Progress review with surgeon. Continued use of compression bandage and taping. Now able to undertake activity to comfort and usually able to get back to most activities. Completely healed with minimal swelling.
Week 6- Progress review with surgeon and return to all activity as comfortable. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Pain should have resolved and minimal swelling is likely to be present.
When a hammertoe is only partially flexible or you have irritation from corns in between your toes, a different procedure is undertaken. Usually, a combination of tendon and capsule releases will be undertaken along with one or more bone cuts. This will bring your toe into a corrected position which is then maintained by taping it in the correct position until healed.
This procedure is undertaken via minimal incision or keyhole hammertoe surgery.
Typical recovery is as follows:
Day 1 to week 1- Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild-moderate pain, bruising and swelling is normal.
Week 1 to week 2- Dressings changed and reduced. Minimal activity restricted to home with foot elevation 80% of the time, able to do home-based activity. Continue foot elevation when seated. Mild pain, bruising and swelling is normal.
Week 2 to week 4- Stitches are taken out and compression bandage with corrective taping put in place at week 2. Restricted to activity in the rigid soled post-operative sandal around home as tolerated.
Week 4- Progress review with surgeon and likely transition to joggers allowed. Continued use of compression bandage and taping. Now able to undertake increased activity to comfort but no extended walking or activity. Daily range of motion exercises provided. Able to undertake upper body exercises. Able to return to work if office-based and able to elevate the foot. Minimal pain and mild swelling is normal.
Week 8- Progress review with surgeon and return to all activity as comfortable. Continue compression as required but can now stop taping. Can return to all footwear as tolerated. Pain should have resolved and minimal swelling may occur for up to 12months.
A fixed or rigid hammertoe is often present when there is a long history of this condition. In these cases, a combination of tendon and capsule releases will be undertaken along with one or more bone cuts of the toe as well as the bone before the toe. This will bring your toe into a corrected position which is then maintained usually with an internal fixation device; however, a wire may be used. Taping may also be used to hold it in the correct position until healed.
This procedure is undertaken depending on how your hammertoe presents through an open incision or via minimal incision or keyhole hammertoe surgery.
Typical recovery is as follows:
Day 1 to week 1- Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild-moderate pain, bruising and swelling is normal.
Week 1 to week 2- Dressings changed and reduced. Minimal activity restricted to home with foot elevation 80% of the time, able to do minimal home-based activity. Continue foot elevation when seated. Mild pain, bruising and swelling is normal.
Week 2 to week 4- Stitches are taken out and compression bandage with corrective taping utilised. Restricted to activity in the rigid soled post-operative sandal around home as tolerated. Able to undertake upper body exercises.
Week 4- Progress review with surgeon. Continued use of compression bandage and corrective taping. Daily range of motion exercises provided. Able to return to work if office-based and able to elevate the foot. Minimal pain and mild-moderate swelling is normal.
Week 6- Progress review with surgeon and removal of the wire (if utilised). Likely transition to joggers allowed. Continued use of compression bandage and taping. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal to no pain and mild swelling is normal.
Week 8- Progress review with surgeon and return to all activity, except sport, as comfortable. Continue compression dressings as required. Pain should have resolved and swelling is likely to be present, particularly on increased activity.
Week 12- Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12months.
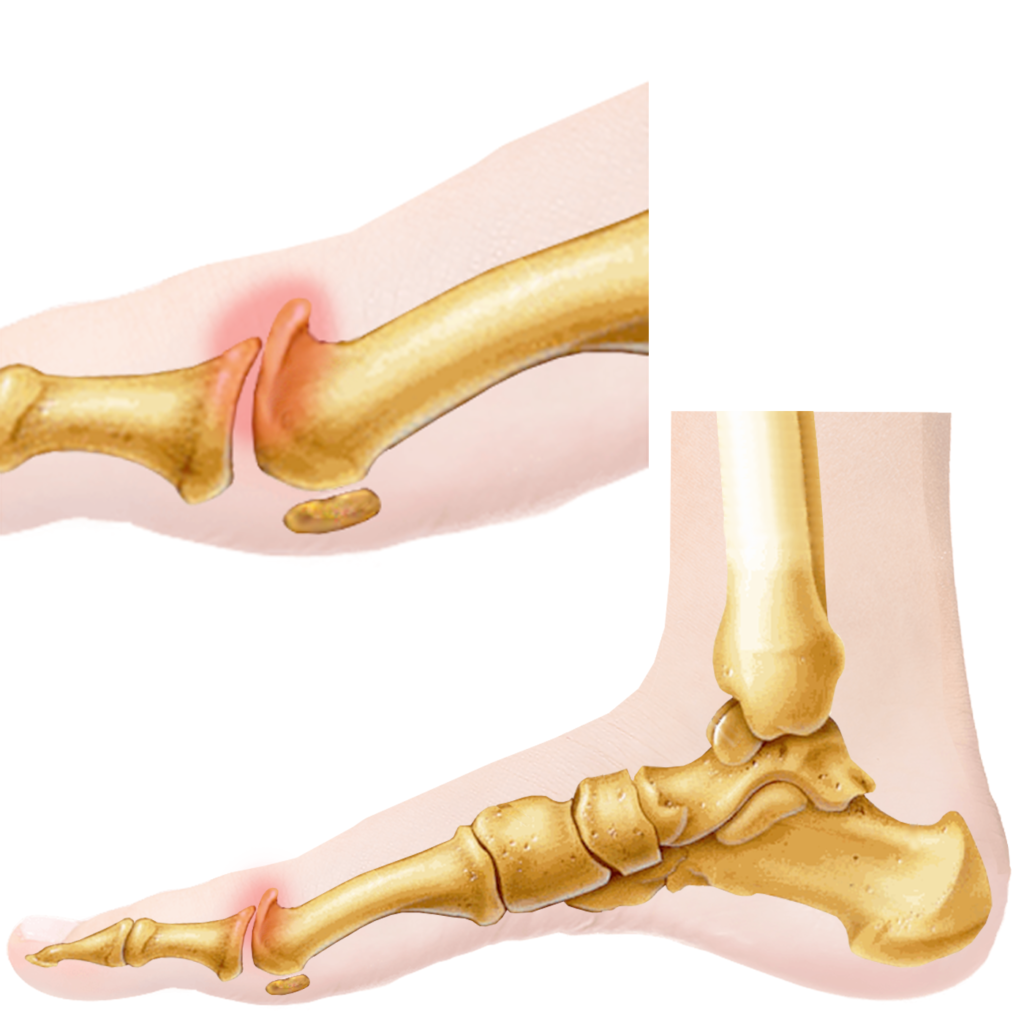
Arthritic Big Toe Joint, AKA, Hallux Limitus and Hallux Rigidus
Hallux limitus and hallux rigidus are conditions that affect the joint at the base of your big toe. They are typically caused from trauma but your genetics may influence your bone structure making your more likely to experience this.
Hallux limitus is a condition where the movement of the big toe gets progressively limited, often due to arthritis or an injury. It can cause pain, especially during activities like walking or running.
If left untreated, it can advance into hallux rigidus, a more severe form of the condition where the big toe becomes extremely arthritic, rigid or even immobile, making walking painful or impossible.
Straight after injury or trauma the toe should be checked with X-rays to make sure there aren’t any fractures or loose pieces of bone. If there is a fracture this will need to be assessed to ensure management is correct for how much injury has happened.
The goal of treatment is to maintain movement. We can decrease how fast your big toe joint arthritis progresses in severity through customised foot orthoses which increase the movement through your big toe joint. They also increase muscle efficiency and spread your body weight throughout your whole foot. They will include accommodations to remove pressure away from prominent or painful areas. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Exercises can help to further increase the range of motion in your big toe. They can also help to strengthen the small muscles within your foot to help support the normal function of your foot. We recommend undertaking big toe joint range of motion exercises, short footing, doming, toe curls and calf stretches.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that your big toe joint arthritis pain may decrease. We recommend joggers or walking shoes when you’re undertaking activity to decrease the pressure on your toes and increase the stability for your big toe joint. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease the pressure on your big toe joint arthritis and increase the efficiency of your lower leg muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing movement at your big toe joint. Another great lacing technique is the ‘bunion step over’. This takes the pressure of the laces off of your big toe joint, decreasing the pain.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
For those who have mild to moderate big toe joint arthritis, or hallux limitus that is not relieved from conservative management, a procedure to remove the extra bone or arthritis will help to decrease pain. This procedure is called a cheilectomy or ostectomy and it is undertaken by minimal incision or keyhole big toe joint surgery. It can also be undertaken open depending on whether there are any fractures or floating bone pieces that need to be removed.
Typical recovery is as follows:
Day 1 to week 1 – Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. A bit more activity up to 20minutes per hour to tolerance but no extended walking or activity. Continue foot elevation when seated. Activity related pain, bruising and swelling is normal.
Week 2 – Stitches are taken out and compression bandage put in place. Daily range of motion exercises provided. Able to undertake upper body exercise. Able to return to work if office-based where you are able to elevate the foot.
Week 4 – Progress review with surgeon and likely transition to joggers allowed. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
When big toe joint arthritis is advanced such as in hallux rigidus, surgery is undertaken to fuse your big toe joint. This procedure is called a joint arthrodesis. The arthritis is removed from the joint and then the big toe is fused so that it won’t move. To fuse the joint there may be screws, fixation plates or wires used to make sure it doesn’t move during healing.
This procedure prevents the painful arthritis from coming back and is a very reliable procedure in advanced stage big toe joint arthritis. By fusing your big toe joint it will change how you walk but most people will find this much more comfortable and happily undertake most sporting activities once recovered.
Typical Recovery is as follows:
Day 1 to week 1 – Dressings in place with a rigid soled post-operative sandal. Minimal activity with the support of crutches. Foot elevation 90% of the time. Mild-moderate pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. Minimal activity restricted to home with foot elevation 80% of the time, able to do minimal home-based activity. Continue foot elevation when seated. Mild pain, bruising and swelling is normal.
Week 2 to week 4 – Stitches are taken out and compression bandage put in place at week 2. Restricted to activity in the rigid soled post-operative sandal around home as tolerated.
Week 4 – Progress review with surgeon. Continued use of compression bandage. Able to return to work if office based where you are able to elevate the foot. Minimal pain and mild swelling is normal.
Week 6 – Progress review with surgeon and likely transition to joggers allowed. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
Sesamoiditis, Sesamoidopathy and Sesamoid Fractures
Sesamoiditis or sesamoidopathy is a condition characterised by inflammation and pain in the sesamoid bones, two small bones embedded in a tendon in the ball of your foot. The condition often results from activities that put strain on these bones, such as running or ballet dancing. The treatment usually includes rest, better footwear, and specific exercises aimed at strengthening the area.
A Sesamoid fracture, on the other hand, is a break in one or both of the sesamoid bones. It’s often caused by trauma, like a fall, or overuse from activities that put pressure on the balls of the feet.

Straight after injury or trauma, the sesamoid bones should be checked with X-rays, ultrasound or MRI to make sure there aren’t any fractures or loose pieces of bone. This also allows us to see whether there is any inflammation around them or whether the bone is getting enough blood to heal. If there is a fracture this will need to be assessed to ensure management is correct for how bad it is.
The goal of treatment is to maintain your movement. Initially, this may mean we need to stop the movement to allow your foot time to heal. We may use splints, taping or a ‘moon boot’ or shoe to stop your big toe joint from moving. We also will take pressure away from the area by putting some padding into your shoes so that when you are walking there is less pressure on the sesamoids.
To make sure that there is as minimal pressure on the sesamoids as possible, customised foot orthoses can be used. They also increase muscle efficiency and spread your body weight throughout your whole foot. They will include accommodations to remove pressure away from prominent or painful areas including the sesamoids. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Once you are recovering and there is less pain, exercises can help to reduce the risk of the pain coming back. They can also help to strengthen the small muscles within your foot to help support the normal function of your foot. We recommend undertaking big toe joint range of motion exercises, short footing, doming, toe curls and calf stretches.
By changing your footwear to a more supportive shoe with a wide and deep toe box you may find that your sesamoid pain may decrease. We recommend joggers or walking shoes when you’re undertaking activity to decrease the pressure on your toes and increase the stability of your whole foot. We realise these may not be as fashionable or stylish for when you are out and about, so in these instances try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease the pressure on your sesamoids and increase the efficiency of your lower leg muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot from sliding forward and aggravating your sesamoids.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
When conservative options fail or you have a severely fractured sesamoid we may need to remove part of or the whole sesamoid. As sesamoids can take a long time to heal due to the small amount of blood flow that they get in some sporting patients, removal of the sesamoid is undertaken sooner. We do this procedure through a small portal on the side or underneath your foot.
Typical recovery is as follows:
Day 1 to week 1 – Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. Minimal activity restricted to home with foot elevation 80% of the time, able to do minimal home-based activity. Continue foot elevation when seated. Mild pain, bruising and swelling is normal.
Week 2 to week 4 – Stitches are taken out and compression bandage put in place at week 2. Restricted to activity in the rigid soled post-operative sandal around home as tolerated.
Week 4 – Progress review with surgeon. Continued use of compression bandage. Transition to joggers allowed. Able to return to work if office-based where you are able to elevate the foot. Minimal pain and mild swelling is normal.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
Morton’s Neuroma
Morton’s neuroma is a painful condition that affects the ball of your foot, most commonly the area between your third and fourth toes. It’s often described as feeling like you have a pebble in your shoe or a fold in your sock.
The condition involves a thickening of the tissue around one of the nerves leading to your toes. This can cause a sharp, burning pain in the ball of your foot and your toes may also sting, burn, or feel numb.

Through the use of padding in your shoes we can help to remove the pressure from the nerve, reducing or resolving the pain. This is typically undertaken through customised foot orthoses which increase muscle efficiency and spreads your body weight throughout your whole foot and away from your pain. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Exercises can help to strengthen the small muscles within your foot taking the pressure away from the nerve. We recommend undertaking short footing, doming, toe curls and calf stretches.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that your Morton’s neuroma will be more likely to be less painful. We recommend joggers or walking shoes when you’re undertaking activity to decrease the pressure on the nerve. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease the pressure on the ball of your foot and increases the efficiency of your lower leg and foot muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot slipping forward.
When other conservative options do not help to relieve pain, a corticosteroid or cortisone injection is provided. This helps to take away the inflammation from the area and as a result the pain. A large percentage of patients will have complete relief of pain, however, some patients will continue to have some pain or reoccurrence of the pain after several months. When this happens, surgical options may be discussed with you.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
Minimal Incision Neuroma Surgery is used to take the pressure away from the nerve. Depending on your imaging results it may be appropriate for you to have a ligament released that holds your metatarsals together. This is a minimal incision or keyhole neuroma surgery technique that means you can get back to your activity quicker.
Typical recovery is as follows:
Day 1 to day 4 – Dressings in place within an appropriate jogger or a rigid-soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Day 4 to Week 2 – Able to remove the dressings and apply a small dressing and compression which is provided. Minimal activity at home with foot elevation when possible, able to do home-based activity. Able to undertake upper body exercises. Able to return to work if office-based and you are able to elevate the foot. Continue foot elevation when seated. Minimal pain, bruising and swelling is normal.
Week 2 to week 4 – Increased activity around home and at work. Stitches are taken out if they were used, and compression bandage applied. Minimal pain and mild swelling is normal.
Week 8 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12months.
When a minimal incision approach is not effective at reducing your pain, the nerve can be removed. This is called a neurectomy. For larger Morton’s neuroma’s, this may be the first option discussed with you to provide the best possible result. This can leave you with some numbness to the toes that the nerve goes to but can completely relieve the pain. This procedure is undertaken through a small portal and recovery is generally quick.
Typical recovery is as follows:
Day 1 to week 1 – Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. Minimal activity restricted to home with foot elevation 80% of the time, able to do minimal home-based activity. Continue foot elevation when seated. Mild pain, bruising and swelling is normal.
Week 2 to week 6 – Stitches are taken out and compression bandage put in place. Restricted to activity in the rigid soled post-operative sandal around the home as tolerated. Able to return to work if office-based and you are able to elevate the foot. Able to undertake upper body exercises. Able to transition to joggers at about week 4.
Week 6 – Progress review with surgeon and transition to joggers allowed if you are not already in them. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
Often Morton’s neuromas are due to other changes in your foot such as bunions and hammertoes. It may also be due to having a longer metatarsal bone than normal. In these cases, surgery may be undertaken to reduce the pressure due to these concerns.
For those who have a longer metatarsal than normal, a careful review of your X-rays may indicate that one or more of these may need shortening. In this case, the procedure is undertaken in a similar fashion to a fixed or rigid hammertoe.
Ingrown Toenail
An ingrown toenail is a common condition where the corner or side of a toenail grows into the soft flesh of the toe, resulting in pain, redness, swelling, and sometimes an infection. It usually affects the big toe, either on one or both sides of the toe.
Several factors can contribute to the development of an ingrown toenail, including improper trimming of the toenails (not straight across), wearing shoes that crowd the toenails, injury to the toenail, and having naturally curved toenails.

A podiatrist can cut your nails for you which will stop an ingrown toenail from digging in and potentially from reoccurring. This is generally pain-free and should allow your nail to start growing out in a more normal way. Often this can help when undertaken every 6-8 weeks in people that often get ingrown toenails who are not appropriate for, or do not wish to have, surgery.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that you are less likely to have pain from, and cause future, ingrown toenails. We recommend joggers or walking shoes when you’re undertaking activity to decrease the pressure on the toenails. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease the pressure on your toenails and increases the efficiency of your lower leg and foot muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot slipping forward and traumatising your nails. Particularly for marathon runners, this is a very helpful technique.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
A partial nail avulsion or removal of the side of the nail is undertaken for ingrown toenails that often get infected or are likely to continue causing pain. This in-office procedure is easily undertaken with local anaesthetic in the chair with a very quick and minimally painful recovery. This is generally undertaken in a way that stops the nail from regrowing where it has been removed from.
Typical recovery is:
Day 1 to day 4 – Dressings in place whilst wearing open-toed footwear. Minimal activity restricted to home for the first 24hours with foot elevation 90% of the time before going back to normal activities after day 1. Mild pain, bruising and swelling is normal.
Day 4 to Week 2 – Able to remove the dressing daily and apply a small dressing. Able to do most home and work-based activity. Minimal pain, bruising and swelling is normal.
Week 2 – Should be healed and able to return to all activity as tolerated. Able to return to enclosed footwear.
Week 8 – Progress review with surgeon. Should have a new nail growing through with no concerns.
A total nail avulsion or total removal of the nail is undertaken particularly when there is a lot of pain and discomfort experienced due to a thickened or fungal infected nail. This procedure is often undertaken as part of a treatment for fungal nails. This can be undertaken to allow the nail to regrow as well as to prevent it from regrowing again.
Typical recovery is:
Day 1 to day 4 – Dressings in place whilst wearing open-toed footwear. Minimal activity restricted to home for the first 24hours with foot elevation 90% of the time before going back to normal activities after day 1. Mild pain, bruising and swelling is normal.
Day 4 to Week 2 – Able to remove the dressing daily and apply a small dressing. Able to do most home and work-based activity. Minimal pain, bruising and swelling is normal.
Week 2 – Should be healed and able to return to all activity as tolerated. Able to return to enclosed footwear.
Week 8 – Progress review with surgeon. Should have a new nail growing through with no concerns.
The Winograd procedure is reserved for ingrown toenails that have excess tissue around them, have a history of recurrence after a partial nail avulsion or are likely to regrow due to the nail shape. During this procedure, a small section of skin is removed with the nail down to the bone. This procedure allows for the removal of where the nail is growing from, called the nail matrix. The skin is then sutured back together. This offers a much better success rate whilst also decreasing some risks around reoccurring ingrown toenails and also reducing the healing time.
Typical recovery is:
Day 1 to day 4 – Dressings in place whilst wearing open-toed footwear. Minimal activity restricted to home for the first 24hours with foot elevation 90% of the time before back to normal activities after day 1. Mild pain, bruising and swelling is normal.
Day 4 to Week 2 – Able to remove the dressing daily and apply a small dressing. Able to do most home and work-based activity. Minimal pain, bruising and swelling is normal.
Week 2 – Sutures are removed and able to return to all activity as tolerated. Able to return to enclosed footwear as tolerated.
Week 8 – Progress review with surgeon. Should have no concerns.
Bone Spurs
Bone spurs, also known as osteophytes, are bony projections that form along the edges of bones. They often develop where bones meet each other in your joints, but they can also appear on the bones of your spine and in your feet, particularly in your heel or around your toes. Corns on toes, subungual exostosis, osteochondromas, and heel spurs are all conditions that can be related to or cause bone spurs in the feet.
Corns on toes are thickened areas of skin that occur in response to excessive pressure and friction. They can sometimes be associated with bone spurs when the spur causes abnormal pressure or rubbing against shoes or neighbouring toes.
Subungual exostosis is a type of bone spur that occurs under the nail, usually the big toe. It often appears as a result of trauma or chronic irritation from tight shoes.
Osteochondromas are benign bone tumors that can cause bone spurs. They most commonly occur in the long bones of the body, but can also appear in the foot such as under your big toenail.
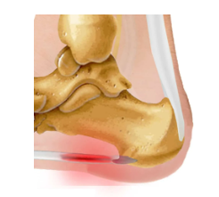
Heel spurs, a specific type of bone spur, occur on the underside of the heel bone and are often associated with plantar fasciitis, a condition that causes inflammation of the band of tissue that runs across the bottom of your foot. They can also be at the back of the heel within the Achilles tendon and are commonly present when you have tight calfs.

We can help to remove the pressure from the bone spur, reducing or resolving the pain. This can be undertaken through removable toe separators, and guards, as well as through customised foot orthoses. This way we can accommodate your bone spur. Orthoses will also help to increase the efficiency of your lower leg and foot muscles whilst spreading your body weight throughout your whole foot and away from your pain. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you may find that you experience less pain. We recommend joggers or walking shoes when you’re undertaking activity to decrease the pressure on bone spurs. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help increase the efficiency of your lower leg and foot muscles and stop your foot from rubbing. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet. It will also help to prevent your feet from slipping forward.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
Corns underneath the foot or in between toes that are not effectively managed with conservative treatments can be managed by removing arthritic bone spurs. We have more information on surgical options for fixing toe arthritis due hammertoes. When corns and pressure areas from this arthritis are not managed they can lead to wounds and ulcers on the bottom of the foot and between toes. Having these treated early is important.
A subungual exostosis is where the bone is prominent underneath the toenail. Using X-rays and by sending the bone for testing we exclude it from being an osteochondroma. Osteochondromas are benign slow-growing bone growths and are very common in the foot. Commonly we see osteochondromas underneath the big toenail in a similar way as a subungual exostosis. When these occur we use a small portal to remove the bone spur, preventing it from coming back. Most people are able to get back to activity quickly.
Typical recovery is:
Day 1 to week 1 – Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. Minimal activity restricted to home with foot elevation 80% of the time, able to do minimal home-based activity. Continue foot elevation when seated. Mild pain, bruising and swelling is normal.
Week 2 to week 6 – Stitches are taken out and compression bandage put in place. Restricted to activity in the rigid-soled post-operative sandal around the home as tolerated. Able to return to work if office-based and you are able to elevate the foot. Able to undertake upper body exercises. Able to transition to joggers as tolerated at week 4.
Week 6 – Progress review with surgeon and transition to joggers allowed if you are not already in them. Continued use of compression bandage. Now able to undertake increased activity to comfort. Minimal pain and mild swelling is normal.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
Heel spurs can be at the bottom, or the back, of the heel bone. These are commonly found with heel pain such as plantar fasciitis and Achilles tendon conditions. A lot of the time, the bone spur is not the cause of pain which is more often due to the tight muscles or not enough strength through your lower leg and foot. We have more information on bottom of heel spurs and heel pain and back of heel spurs and Achilles tendon conditions.
Flat Feet
Flat feet, or pes planus, occurs when the arches of the feet flatten, allowing the entire sole to touch the ground when standing. This condition can be congenital or develop over time due to factors like aging, injuries, or certain medical conditions like diabetes or rheumatoid arthritis. While many individuals with flat feet experience no discomfort, some may experience pain in the feet, ankles, lower legs, knees, hips, or lower back, particularly during physical activity.

Through customised foot orthoses we can increase muscle efficiency and spread your body weight throughout your whole foot. They will bring your foot into a more efficient position and take pressure away from prominent or painful areas. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Exercises can help to strengthen the small muscles within your foot to help support the normal function of your foot. We recommend undertaking short footing, doming, toe curls and calf stretches.
By changing your footwear to supportive shoes you will find decreased pain due to having flat feet. We recommend joggers or walking shoes when you’re undertaking activity to spread pressure evenly throughout your feet. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help increase the efficiency of your lower leg and foot muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing injury.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
Minimal Incision flat foot surgery is a great option to prevent flat foot related pain. It has also been shown to be effective in reducing mild bunions, heel pain and tarsal tunnel syndrome and arthritis. Minimal incision or keyhole flat foot surgery is undertaken by placing a stent called HyproCure into a joint in your rearfoot. It looks like a screw and sits in place to make your joint work like a saddle. It works with your foot to prevent your foot from flattening and is sized during the procedure to ensure correct fitting.
Typical recovery is as follows:
Day 1 to week 1- Dressings in place with a rigid soled post-operative sandal or CAM boot. Use of crutches for all walking. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2- Dressings changed and reduced. A bit more activity up to 20minutes per hour to tolerance but no extended walking or activity. Continue foot elevation when seated. Activity related pain, bruising and swelling is normal.
Week 2- Stitches are taken out and compression bandage put in place. Able to walk without crutches. Daily range of motion exercises provided. Able to undertake upper body exercise. Able to return to work if office-based and where you are able to elevate the foot.
Week 4- Progress review with surgeon and likely transition to joggers allowed. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 12- Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12months.
Foot Arthritis
Foot arthritis is a condition that causes inflammation, pain, and swelling in the joints of the foot. There are different types of foot arthritis, including osteoarthritis, rheumatoid arthritis, and gout.
Osteoarthritis is the most common type, often affecting older adults due to wear and tear over time. Symptoms include stiffness and pain in the foot and ankle joints.
Rheumatoid arthritis (RA) is a systemic inflammatory disease that may affect multiple joints leading to inflammation, pain, stiffness, and swelling. It can cause soreness, warmth, and swelling of one or more foot joints.
Foot arthritis can limit mobility and affect a person’s daily life. It can cause pain and swelling in the foot, ankle, legs, and back.

X-rays are used to see the extent of arthritis and to make sure there aren’t any fractures or loose pieces of bone. If there is a fracture this will need to be assessed to ensure management is correct for how much injury has happened. Often we find X-rays show us everything we need, but we may need to send for an ultrasound, CT or MRI.
The goal of treatment is to reduce pain and where possible maintain movement. We can decrease how fast your arthritis progresses in severity through customised foot orthoses. They increase muscle efficiency and spread your body weight throughout your whole foot, taking the pressure off arthritic joints. They will include accommodations to remove pressure away from prominent or painful areas. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Exercises can help to further maintain the range of motion in your foot. They can also help to strengthen the small muscles within your foot to help support the normal function of your foot. We recommend undertaking big toe joint range of motion exercises, short footing, doming, toe curls and calf stretches.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that your arthritis pain may decrease. We recommend joggers or walking shoes when you’re undertaking activity to decrease the pressure on your toes and increase your stability. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease the pressure on any arthritis and increase the efficiency of your lower leg muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot from slipping in your shoe. Another great lacing technique for those who have bunions or big toe joint arthritis is the ‘bunion step over’. This takes the pressure of the laces off of your big toe joint, decreasing the pain.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
When other conservative options do not help to relieve pain, a corticosteroid or cortisone injection is provided. This helps to take away the inflammation from the area and as a result the pain. Some patients will have complete relief of pain, however, other patients will continue to have some pain or reoccurrence of pain after several months. When this happens, surgical options may be discussed with you.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
Arthritis of the big toe joint can cause painful rubbing and decreased movement. This can be caused by trauma from osteoarthritis, gout or other conditions that affect the foot. Arthritis of the big toe joint is typically called hallux limitus when the big toe can still move and hallux rigidus when the big toe doesn’t move at all.
Hallux limitus can progress to hallux rigidus, so undertaking assessment, diagnosis and appropriate treatment as soon as you injure it or as soon as you notice pain or decreased movement will give you the best possible longer-term outcome. Find more information on hallux limitus and hallux rigidus now.
Hammertoe, claw toe, curly toe, mallet toe. These are all names for toes that are bending in different directions due to arthritis. They can cause corns and callus on top, on the sides and at the end of the toes. At times these may cause wounds and become ulcers.
Generally, hammertoes are caused by repetitive trauma either at a joint or on the plantar plate. The plantar plate is a ligament underneath the ball of the foot and when traumatised, known as a plantar plate tear, it can cause the toe to stick up and the toe joints to change their position into a flexed position. Hammertoes can be caused over time due to bunions and weakness in the small muscles in your feet. They may also be caused by other conditions like Morton’s neuroma.
Hammertoe deformities can be progressive, so undertaking assessment, diagnosis and appropriate treatment as soon as you injure it or as soon as you notice the deformity will give you the best possible longer-term outcome. Read more information on hammertoes now.
When there are multiple deformities or problems of the forefoot we occasionally need to do several surgeries at one time to provide the best outcome for you. This often happens in people who have had rheumatoid arthritis for a long time or those who have bunions, hammertoes and arthritis. When these conditions are treated at the same time a very individual surgical plan is created based on your concerns, medical history and imaging. Due to this, appropriate consultation is required before conservative and surgical options can be suggested.
Heel Pain, Plantar Fasciitis and Tarsal Tunnel Syndrome
Plantar Fasciitis is a common foot condition that results in pain in the heel and bottom of the foot. It occurs when the plantar fascia, a thick band of tissue that runs across the bottom of your foot and connects your heel bone to your toes, gets inflamed. This inflammation causes intense discomfort, particularly upon waking up or after periods of sitting or standing for a long time.
Tarsal Tunnel Syndrome, on the other hand, is a condition that arises from the compression of the posterior tibial nerve as it travels through the tarsal tunnel, a narrow passageway inside your ankle. This pressure on the nerve can lead to various symptoms like burning sensations, tingling, numbness, and pain in the ankle and the sole of the foot. The exact reason behind Tarsal Tunnel Syndrome is often hard to identify, but it can be associated with factors such as flat feet, systemic diseases like diabetes, or an injury to the nerve.

Ultrasound and X-rays in combination with a thorough assessment are used to help ensure that we are providing the best treatment. Often we find ultrasounds and X-rays show us everything we need, but occasionally we may need to send for an MRI to get an even better look at what is happening.
The goal of treatment is to reduce pain and where possible maintain movement. We can decrease your heel pain through customised foot orthoses. They increase muscle efficiency and spread your body weight throughout your whole foot, taking the pressure off of injured areas. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Exercises can help to further maintain the strength and range of motion in your foot. They can also help to strengthen the small muscles within your foot to help support the normal function of your foot. We recommend undertaking big toe joint range of motion exercises, short footing, doming, toe curls and calf stretches.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that your heel pain may decrease. We recommend joggers or walking shoes when you’re undertaking activity to spread the pressure more evenly through your feet. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease your pain and increase the efficiency of your lower leg muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot from slipping in your shoe.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
When other conservative options do not help to relieve pain, a corticosteroid or cortisone injection is provided. This helps to take away the inflammation from the area and as a result the pain. A large percentage of patients will have complete relief of pain, however, some patients will continue to have some pain or reoccurrence of pain after several months. When this happens, surgical options may be discussed with you.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
Achilles Tendon Conditions
The Achilles tendon is a band of tissue that connects calf muscles to the heel bone. It’s the largest tendon in the body and plays a crucial role in basic activities like walking, running, and jumping. Common conditions affecting the Achilles tendon include tendinitis, peritendonitis, tendinosis, rupture, and retrocalcaneobursitis. Achilles tendinitis is a common condition that occurs when this tendon becomes irritated and inflamed, causing pain and swelling in the back of the leg or above the heel.

Ultrasound and X-rays in combination with a thorough assessment are used to help ensure that we are providing the best treatment. Often we find ultrasounds and X-rays show us everything we need, but occasionally we may need to refer for an MRI to get an even better look at what is happening.
The goal of treatment is to reduce pain and maintain movement. We can decrease your pain through customised foot orthoses. They increase muscle efficiency and spread your body weight throughout your whole foot, taking the pressure off of injured areas. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Exercises can help to further maintain the strength and range of motion in your foot. They can also help to strengthen the small muscles within your foot to help support the normal function of your foot. We recommend undertaking calf strengthening, short footing, doming and toe curls.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that your pain may decrease. We recommend joggers or walking shoes when you’re undertaking activity to spread the pressure more evenly through your feet. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease your pain and increase the efficiency of your lower leg muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot from slipping in your shoe.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
Achilles tendon injuries can be small tears through to complete rupture of the tendon. Depending on how damaged your tendon is and whether there are other conditions occurring, we treat you with as minimally invasive a procedure as possible. This may mean we remove some tendon during an open procedure or reattach your tendon to the heel bone. In some cases, other tendons are required to be attached to your Achilles tendon to ensure that you have the strength to get back to the majority of your activities.
Due to the variance in procedures and individual factors, there is no typical recovery rate but most people are walking unaided at six weeks and are able to start reintroducing exercises that lead to sports by twelve weeks. Full return to sport may take up to twelve months.
At times a minimal incision or keyhole heel spur removal is undertaken. This procedure is used when there is an elongated or fractured heel spur that is likely to be causing some of your pain in addition to the Achilles tendon pain. Typically patients will have a large bump at the back of their heel which is painful in shoes and may have blisters due to rubbing. Minimal incision or keyhole heel spur removal is undertaken to reduce the bone spur prominence and associated pain.
Typical recovery is as follows:
Day 1 to week 1 – Dressings in place with a rigid soled CAM or ‘Moon’ boot. Crutches are used when walking around. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. A bit more activity up to 20minutes per hour to tolerance but no extended walking or activity. Continue foot elevation when seated. Activity related pain, bruising and swelling is normal.
Week 2 – Stitches are taken out and compression bandage put in place. Daily range of motion exercises provided. Able to undertake upper body exercise. Able to return to work if office-based and where you are able to elevate the foot.
Week 6 – Progress review with surgeon. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12months.
Foot Fractures and Stress Fractures
A foot fracture refers to an injury where one or more of the bones in the foot breaks. This can occur due to various reasons such as a car crash, a simple misstep, a fall, or a sports injury. In some cases, it could also be the result of overuse and repetitive activity leading to stress fractures.
Stress fractures are a specific type of foot fracture. They are small cracks in a bone, or severe bruising within a bone, typically caused by overuse and repetitive activity.

X-rays are used to see how bad the fracture is. If there is a fracture this will need to be assessed to ensure management is correct for how much injury has happened. Often we find X-rays show us everything we need, but occasionally we may need to send for an ultrasound, CT or MRI to rule out any injury to other areas of your foot.
The goal of treatment is to allow the fracture to heal. To do this we usually need to stop any movement happening around the fracture. We can increase how fast your fracture heals by stopping movement with the use of a CAM boot or shoe with appropriate offloading placed into it. This will remove pressure away from your fracture, increasing the bodies ability to heal.
Fractures are usually due to overloading. Due to this, we can target any overloaded areas of your foot through customised foot orthoses. They increase muscle efficiency and spread your body weight throughout your whole foot, taking the pressure off any fractured or high-pressure areas. They will include accommodations to remove pressure away from prominent or painful areas. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Exercises can help to further maintain the range of motion in your foot. They can also help to strengthen the small muscles within your foot to help support the normal function of your foot. Once you have been given the okay to start your rehabilitation, we recommend undertaking big toe joint range of motion exercises, short footing, doming, toe curls and calf stretches.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that there is less pressure on your feet. We recommend joggers or walking shoes when you’re undertaking activity to decrease the pressure on your toes and increase your stability. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease the pressure on specific areas of your foot and increase the efficiency of your lower leg muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot from slipping in your shoe.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
Metatarsals are bones that are commonly fractured in the foot. They are the bones that connect to your toes and make up the forefoot of your feet.
More often we see metatarsal stress reactions which can be caused due to increased activity or starting high load activities such as a new gym program without undertaken appropriate strengthening. When metatarsal fractures occur we undertake X-rays to see whether you will heal without surgery.
In cases where there is too much movement of the bone or if it is unlikely to heal, we will suggest a surgical option. Sometimes, we are able to undertake a minimal incision reduction of the fracture but at times we may need to undertake an open reduction of the fracture.
Toe fractures can be painful but despite their pain, they generally don’t need surgery. Longer-term these fractures can cause arthritis and clawing of the toes such as hammertoes. An X-ray will indicate what treatment is necessary and appropriate management will be undertaken. Unless it is severely malpositioned, usually a period in an offloading shoe will help it to heal.
Sesamoid fractures are caused by a single significant force such as landing on it wrong when jumping from height or from multiple small forces that occur quicker than what the sesamoid can heal itself. Find out more about sesamoid conditions and fractures now.
Accessory Ossicles
Accessory ossicles are extra bones that are present at birth. They are not part of the normal skeleton and are typically found in areas where a bone might have split into two separate parts during early development. These are most commonly found in the foot and ankle.
While they don’t usually cause any problems, sometimes they can become painful or uncomfortable, especially if they’re injured or inflamed.

X-rays are used to see how your bones are positioned and to confirm your diagnosis. If there is an ossicle the X-ray will show us where it is and what type of ossicle it is. This will need to be assessed to ensure management is correct for how to reduce pressure. Often X-rays do not show us everything and so we may need to send for an ultrasound, CT or MRI to make sure we can see exactly what is happening in your foot.
Initially, the goal of treatment is to reduce the inflammation that is occurring to the ossicle. We can do this through the use of a moon boot or special shoe with custom pressure offloading placed into them. This will remove pressure away, increasing the body’s ability to heal.
We often find that pain from accessory ossicles is due to decreased muscle strength and how we walk. We can reduce these concerns through customised foot orthoses. They increase muscle efficiency and spread your body weight throughout your whole foot, taking the pressure off the ossicle. They will also include accommodations to remove pressure away from prominent or painful areas. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that there is less pressure and greater muscle efficiency for your feet. We recommend joggers or walking shoes when you’re undertaking activity to decrease the pressure on your toes and increase your stability. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease the pressure on specific areas of your foot and increase the efficiency of your lower leg muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot from slipping in your shoe.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
The os peroneum is found in a large proportion of the population with estimates ranging up to 26% of people. This accessory ossicle is located on the outside of the midfoot within the peroneal longus tendon and commonly causes pain when walking and jogging. Some patients will injure their os peroneum when they have an ankle sprain and so ensuring the correct diagnosis is essential to managing ongoing painful ankle sprains.
This condition can usually be resolved successfully with conservative treatment but when this fails, surgical removal of the accessory bone and repair of the tendon usually resolves the pain.
Typical recovery is:
Day 1 to week 1 – Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. A bit more activity up to 20minutes per hour to tolerance but no extended walking or activity. Continue foot elevation when seated. Activity related pain, bruising and swelling is normal.
Week 2 – Stitches are taken out and compression bandage put in place. Daily range of motion exercises provided. Able to undertake upper body exercise. Able to return to work if office-based and where you are able to elevate the foot.
Week 4 – Progress review with surgeon. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 6 – Progress review with surgeon and return to joggers. increased activity as comfortable. Continue compression. Pain should have resolved and swelling is likely to be present, particularly on increased activity.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
Found in up to 14% of the population this bone is a very common accessory ossicle. It is located on the inside of your foot, just above the middle of your arch. Typically we can see a prominence which alerts us to the likelihood of this and so guides us to undertake x-rays to confirm our clinical findings.
This accessory ossicle typically leads to decreased strength of the muscles that hold up the arch and so is found in patients who have flat feet more often. Although this ossicle responds very well to rest and other conservative treatments, at times surgery may be required.
When surgery is required, a full assessment is undertaken to gain a further understanding of the most appropriate way to undertake the surgery. Typically removal of the ossicle and repair of the tendon is undertaken however due to there being many different subtypes of this ossicle, individual assessment and management are required.
Typical recovery is:
Day 1 to week 1 – Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. A bit more activity up to 20minutes per hour to tolerance but no extended walking or activity. Continue foot elevation when seated. Activity related pain, bruising and swelling is normal.
Week 2 – Stitches are taken out and compression bandage put in place. Daily range of motion exercises provided. Able to undertake upper body exercise. Able to return to work if office-based and where you are able to elevate the foot.
Week 4 – Progress review with surgeon. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 6 – Progress review with surgeon and return to joggers. increased activity as comfortable. Continue compression. Pain should have resolved and swelling is likely to be present, particularly on increased activity.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
The os trigonum accessory ossicle is found in about 7% of the population and is located on the back of the foot and deep to the Achilles tendon. This little bone is commonly painful in ballet dancers who are en pointe and in those who have a trauma that results in their toes being pointed suddenly down.
After diagnosis, this condition will generally respond well to conservative treatment. When surgery is required a simple removal of the os trigonum is usually successful in resolving pain and enabling a return to activity.
Typical recovery is:
Day 1 to week 1 – Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. A bit more activity up to 20minutes per hour to tolerance but no extended walking or activity. Continue foot elevation when seated. Activity related pain, bruising and swelling is normal.
Week 2 – Stitches are taken out and compression bandage put in place. Daily range of motion exercises provided. Able to undertake upper body exercise. Able to return to work if office-based and where you are able to elevate the foot.
Week 4 – Progress review with surgeon. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 6 – Progress review with surgeon and return to joggers. increased activity as comfortable. Continue compression. Pain should have resolved and swelling is likely to be present, particularly on increased activity.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
Warts and Verruca Pedis
Verruca Pedis, also known as plantar warts, are small growths that usually appear on the heels or other weight-bearing areas of your feet. They’re caused by the human papillomavirus (HPV), which enters your body through tiny cuts and breaks in your skin.
Plantar warts can be painful when you squeez them and with direct pressure like when you’re standing or walking.

As warts are caused by viruses, treatment aims to activate the immune system. This is generally achieved by causing a local irritation to the area using tapes, mild acids and trauma. Commonly pharmacists can supply ointments that contain salicylic acid. You may also find that freezing the lesion helps to resolve it as well due to the cold creating a blister. At Relieve Health Group we use a number of different options depending on the patients’ age, activities and pain level.
More recently, treatment using microwave therapy can be undertaken. This is not something that is undertaken at Relieve Health Group but can be trialled in patients wishing to avoid surgery.
The wart curettage procedure is undertaken under local anaesthetic to remove the viral wart tissue entirely, preventing the wart from returning.
This procedure is undertaken in the clinic and requires you to be in a special shoe during recovery for up to three weeks. This is the preferred option in surgically managing stubborn warts.
This technique causes multiple punctures of the wart area in order to create an immune response to the wart. Over a period of three months, the immune system will likely resolve the warts on your feet.
This procedure is undertaken when minimal time off of your feet is required and can be undertaken in the clinic under local anaesthetic.
Ganglionic Cysts
Ganglionic cysts are lumps that most commonly develop along the tendons or joints. These cysts are filled with a jellylike substance that comes from the tissue lining the joint or tendon.
The size of ganglionic cysts can vary, and they might get larger when you use that joint for repetitive motions. They’re usually painless, but if a cyst presses on a nerve, it can hurt, cause muscle weakness, or tingling.
The exact cause of ganglionic cysts is unknown, but they may occur due to injury or overuse of a joint.
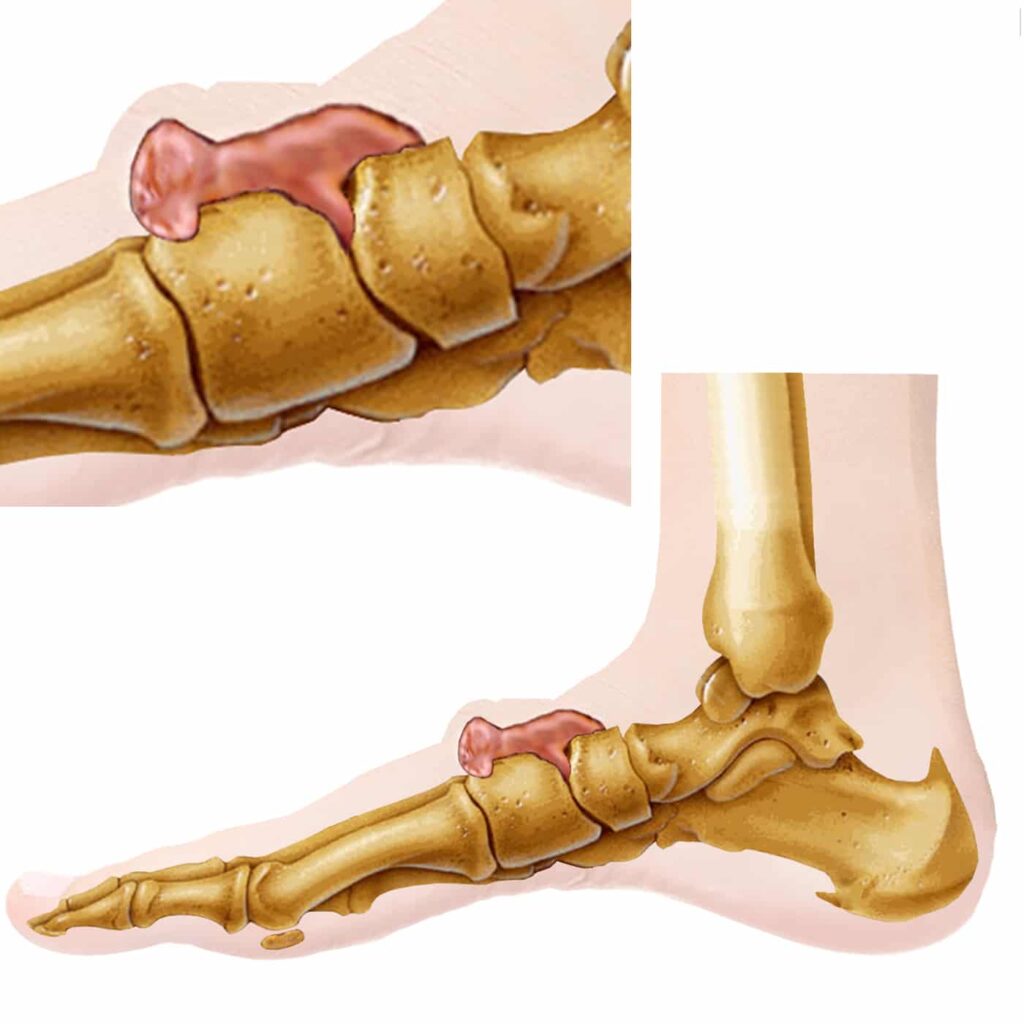
Ultrasound and sometimes X-rays in combination with a thorough assessment are used to help ensure that we are providing the best treatment. Often we find ultrasounds and X-rays show us everything we need, but occasionally we may need to send for an MRI to get an even better look at what is happening.
The goal of treatment is to reduce pain and where possible maintain movement. We can decrease your pain associated with ganglionic cysts through customised foot orthoses. They increase muscle efficiency and spread your body weight throughout your whole foot, taking the pressure off of injured areas. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Exercises can help to further maintain the muscle strength and range of motion in your foot. They can also help to strengthen the small muscles within your foot to help support the normal function of your foot. We recommend undertaking big toe joint range of motion exercises, short footing, doming, toe curls and calf stretches.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that your ganglionic cyst pain may decrease. We recommend joggers or walking shoes when you’re undertaking activity to spread the pressure more evenly through your feet. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear.
Changing your shoe lacing will help decrease your pain and increase the efficiency of your lower leg muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot from slipping in your shoe.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
When other conservative options do not help to relieve pain, a corticosteroid or cortisone injection is provided. This helps to take away the inflammation from the area and as a result the pain. A large percentage of patients will have complete relief of pain, however, some patients will continue to have some pain or reoccurrence of pain after several months. When this happens, surgical options may be discussed with you.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
When conservative options fail and you are having considerable pain, surgical options may be discussed. Surgical approaches will depend on where and how large the ganglionic cyst is.
When surgery is required, a full assessment is undertaken to gain an understanding of the most appropriate way to undertake your individual surgery. For further information please make an appointment.
Typical recovery is:
Day 1 to week 1 – Dressings in place with a rigid soled post-operative sandal. Minimal activity restricted to home with foot elevation 90% of the time. Mild pain, bruising and swelling is normal.
Week 1 to week 2 – Dressings changed and reduced. A bit more activity up to 20minutes per hour to tolerance but no extended walking or activity. Continue foot elevation when seated. Activity related pain, bruising and swelling is normal.
Week 2 – Stitches are taken out and compression bandage put in place. Daily range of motion exercises provided. Able to undertake upper body exercise. Able to return to work if office-based and where you are able to elevate the foot.
Week 4 – Progress review with surgeon and likely transition to joggers allowed. Continued use of compression bandage. Now able to undertake increased activity to comfort but no extended walking or activity. Minimal pain and mild swelling is normal.
Week 12 – Progress review with surgeon. No longer requires compression bandage. Able to use any footwear as tolerated. Able to build up sports and activities as tolerated. Mild swelling may occur for up to 12 months.
Pressure Ulcers
Foot ulcers may be related to diabetes or poor feeling or blood flow. These ulcers form over areas of bony prominences, especially when conditions like bunions, calluses or hammer-toe formations lead to increased pressure. They are a common reason for hospital stays among people with diabetes, and their healing process may take weeks, several months or even years.
The top five causes of diabetic foot ulcers include high blood sugar levels, poor circulation, nerve damage, immune system issues, and deformities. High blood sugar levels can cause damage to both nerves and blood vessels, which can lead to decreased sensation and poor blood flow in the feet. This can make it difficult for individuals to notice minor cuts, scrapes, or pressure sores. Poor circulation makes it harder for these wounds to heal. Over time, unhealed wounds can develop into ulcers.

X-rays are used to see how your bones are positioned and to ensure there is no bone infection. They are also used to compare your foot to how it looked previously and in the future so that we can see if it is changing. If there is a prominent area this will need to be assessed to ensure management is correct in how to reduce this pressure. Often we find X-rays show us everything we need, but occasionally we may need to send for an ultrasound, CT or MRI to rule out any injury or concerns to other areas of your foot. We will also work with your entire health team to ensure you get the most appropriate care possible. This may include referral to a vascular (blood) specialist, endocrinologist (diabetes specialist) or neurologist (nerve specialist).
The goal of treatment is to remove all pressure from any wounds or pressure areas. We can do this through the use of a moon boot or special shoe with custom pressure deflection placed in it. This will remove pressure away from your wound or pressure area, increasing the body’s ability to heal.
Pressure areas can be made worse by abnormal walking. Due to this, we can target how you are walking to decrease high-pressure areas on your foot through customised foot orthoses. They increase muscle efficiency and spread your body weight throughout your whole foot, taking the pressure off any wounds or high-pressure areas. They will include accommodations to remove pressure away from prominent or painful areas. These are purchased on assessment and recommendation by your local podiatrist and are customised individually for each one of your feet.
Further pressure can be removed from your wound or pressure area by removing the dead skin around it. This is commonly known as callus and is hard skin that can sometimes be soft due to increased moisture from your ulcer. Through the removal of this dead skin back to healthy skin, there is less pressure and the ulcer will heal quicker. This can be undertaken by your local podiatrist or on referral to your local public hospital podiatry department.
By changing your footwear to a wide and deep toe box and a soft and flexible upper material you will find that there is less pressure on your feet. We recommend joggers or walking shoes when you’re undertaking activity to decrease the pressure on your toes and increase your stability. We realise these may not be as fashionable or stylish for when you are out and about so in these instances, try to stick to as comfortable a shoe as possible and steer away from high heels or unsupportive footwear. For people with larger pressure areas or with a deformity that prevents them from wearing normal shoes, custom shoes can be made to help you walk better and remove the pressure.
Changing your shoe lacing will help decrease the pressure on specific areas of your feet and increase the efficiency of your lower leg muscles. We recommend to everyone to have loop lock lacing to increase the efficiency of your muscles, spreading the forces more evenly to the bottom of your feet and preventing your foot from slipping in your shoe.
Photobiomodulation therapy (PBMT) uses red and near infrared light to increase the energy in our body (ATP) and reduce free radicals (like nitrous oxide). It allows for increased healing, reduced swelling and reduced inflammation and most importantly reduced pain. It naturally speeds up our body’s normal healing process with no pain during treatment. PBMT is used on all muscle, tendon, nerve, skin and bone injuries. The evidence indicates that we can heal up to 70% faster when using PBMT to increase our healing rate. Research reports exactly what we see in clinic, laser therapies heal nerves and decrease how much pain we feel. For patients who we recommend to undertake PBMT, we undertake treatment with a powerful robotic laser therapy unit. This unit is Italian made out of the Florence University in conjunction with ASA Laser and is called the MLS M8. First consultations are free and can be booked in our rooms with our laser and pain therapists. You can also purchase a laser therapy wrap during your consult to use at home.
You can find videos on all of these options on our MHE Community Hub, our Relieve Health Group Youtube channel or by contacting us in clinic.
When these pressure areas become a significant problem and are not able to be managed effectively through conservative options, surgery may be suggested.
Before surgery is undertaken a thorough assessment of your current health is required. This may involve discussion with your GP and specialists to ensure that surgery is safe for you to undertake.
Depending on where your concern is, anything from a simple one minute procedure that releases pressure on your toe may be able to be undertaken. We also help decrease larger pressure areas by removing bone bumps via minimal incision or keyhole surgery. This will depend on where your problem is and what your anatomy is.
If you have pressure from a bunion or a hammertoe you may find information that can help, however, to learn more about options specific for you, book an appointment.
Revision Surgery
When appropriate revision surgery may be suggested. If surgery is suggested as your best option, it is important to understand that it may not resolve all of your pain or concerns. In these cases, we aim to lessen your concerns as much as possible in order to allow you to undertake as many activities as possible that you were doing before your initial surgery. Depending on the type of procedure undertaken, this may also mean an extended recovery.

Due to the individual nature of this concern, a thorough assessment is undertaken before proposing a diagnosis and appropriate treatment options. This will help to provide the best possible longer-term results.

Specialist Foot Surgeon
Dr. Hungerford Welcomes All Patients, With And Without A Referral, For The Specialist Opinion Of All Foot Conditions. Come Visit Us In Shellharbour City To Get Started With Your Treatment.
Take the First Step Towards Better Health with Relieve Health Group
Ready to prioritise your health? Take the first step towards better well-being with Relieve Health Group. Our compassionate team is here to provide personalised care and support tailored to your needs. Contact us today and experience our exceptional healthcare services. Your health is our priority.
DISCLAIMER: All information on this website is for education purposes only. Individual management plans and recovery may vary depending on your diagnosis, age, health issues and anatomy. Any surgical or invasive procedure carries risks. Before undertaking any treatment, you should seek an opinion from an appropriately qualified health practitioner.